What is Spermatocele?
Spermatoceles are benign cysts of the scrotum. They are very common and more often than not need no treatment. Spermatoceles are not cancerous nor will they become cancerous. They are most often confused with hydroceles, another benign cystic disease of the scrotum.
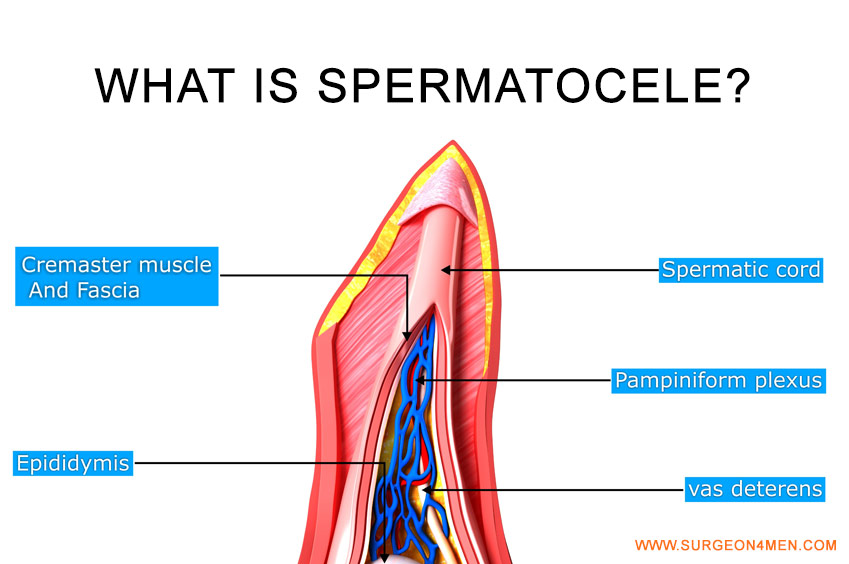
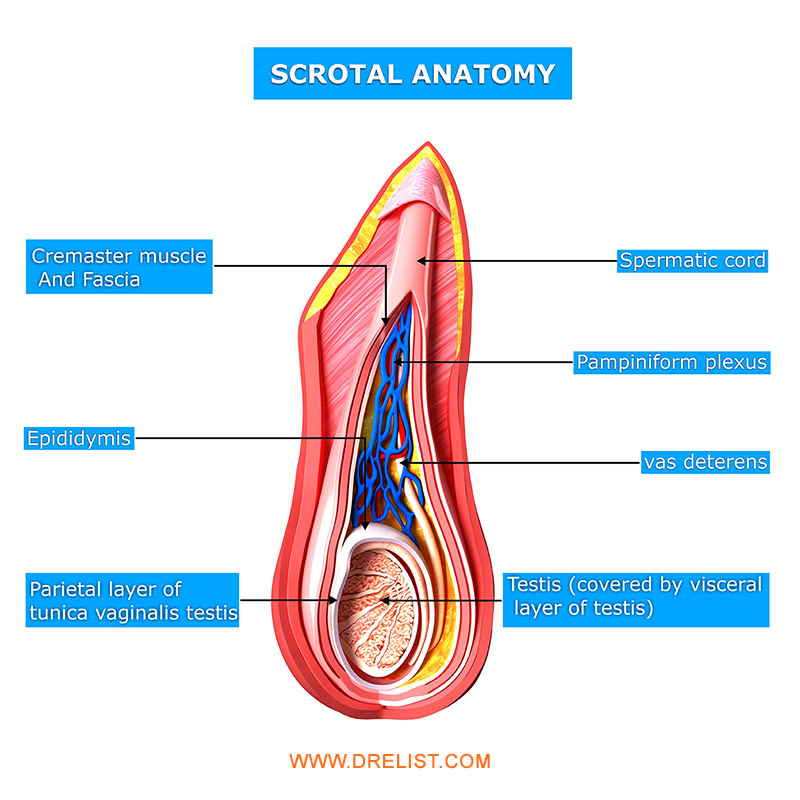
Anatomy
 To understand spermatoceles one must understand the anatomy of the scrotum, or the sac that contains the testicles. Normally every male has two testicles within the scrotum. The testicles’ main functions are to produce the male hormone testosterone and to produce sperm. The hormonal aspects of the testicles are unrelated to spermatoceles. The sperm production aspects are related.
To understand spermatoceles one must understand the anatomy of the scrotum, or the sac that contains the testicles. Normally every male has two testicles within the scrotum. The testicles’ main functions are to produce the male hormone testosterone and to produce sperm. The hormonal aspects of the testicles are unrelated to spermatoceles. The sperm production aspects are related.
After sperm is produced in the testicles they migrate into a gland called the epididymis. The epididymis is a small tubular gland about one and a half inches long and as broad around as a pencil. The epididymis sits behind the testicle and is a series of microscopic tubes that if unfolded would be many hundred feet long. It is here that the sperm, released by the testicle, mature. The maturation process takes about six weeks, and at the end of the epididymis is the vas or vas deferens, the single duct or tube that transports the sperm towards the prostate gland where it will join the seminal fluid that is produced. I might add at this point that sperm is only a small component of semen volume. Most of the fluid that is ejaculated comes from the prostate gland, which is located inside the body beneath the bladder.
Cause of Spermatoceles
The epididymis is the source of spermatoceles. For a number of reasons such as trauma, infection, congenital abnormalities and for no reason at all, one of the tubes of the epididymis no longer transports sperm properly. The end result is a widening of the tube into a small cavity or ‘cyst’. This would be compared to the effects of a dam that creates a lake by obstructing the flow of water. As times goes on the cyst can continue to enlarge. In many instances spermatoceles remain small, less than one-half an inch or so, and when they remain small we usually call them ‘epididymal cysts’. In other instances the spermatoceles continue to enlarge and can become five to six inches or larger in size!
Most of the time spermatoceles are painless. However, they can enlarge enough to make clothing uncomfortable, or at least tight-fitting with certain types of clothing.
Treatment of Spermatoceles
 Spermatoceles do not go away without treatment. Fortunately most spermatoceles require no treatment. If the spermatocele is not causing pain or is not so large that clothing is uncomfortable or unsightly, the spermatoceles can be left alone.
Spermatoceles do not go away without treatment. Fortunately most spermatoceles require no treatment. If the spermatocele is not causing pain or is not so large that clothing is uncomfortable or unsightly, the spermatoceles can be left alone.
If the spermatocele does require treatment, surgical removal is required. Surgery is usually done as an outpatient and requires less than an hour to perform. A general spinal or even local anesthetic can be used for the procedure. Most patients will need to stay off their feet for three to five days and reduce activity for a week.
Risks of the Spermatoceles Surgery
Risks of the surgery include bleeding, pain and infection as is associated with any
surgical procedure. The unique risks include recurrence of the spermatocele. Since the epididymis is left in place there is the possibility of another duct blocking at a later time. The recurrence rate is about 5 percent. If the epididymis is removed with the spermatocele, the recurrence rate is lower, but then there is an slight increase in risk of damage to the blood supply to the testicle.
Because the epididymis is an integral part of the sperm transport system, any surgery done near the epididymis could cause occlusion of the duct similar to having a vasectomy on that side. If fertility is not a concern, then epididymal trauma is not a risk. If the patient is still considering having children, spermatocelectomy should be put off until all childbearing is completed. Hormone problems after spermatocele removal is a very unlikely event and would only occur in the rare event that the blood supply to the testicle is damaged.
If you have any questions about spermatocele or the removal of spermatocele, please don’t hesitate to ask.